The brain-gut axis may be the key to our physical, mental and emotional health
Share
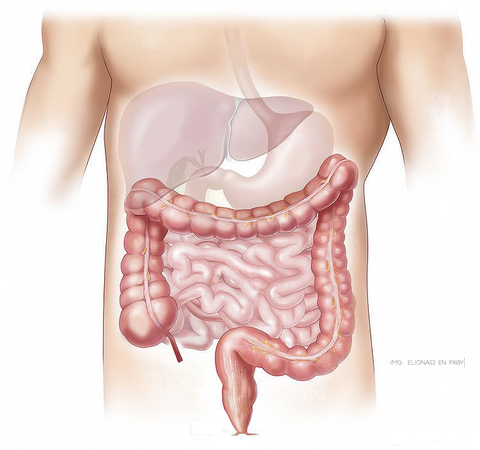
The brain-gut axis (BGA) refers to the bidirectional communication between the central nervous system and the enteric or intestinal system, which links the emotional and cognitive centers of the brain with peripheral intestinal functions.
This two-way communication network includes the central nervous system (CNS), both the brain and spinal cord, the autonomic nervous system (ANS), the enteric nervous system (ENS), and the hypothalamic-pituitary-adrenal axis.
Recent research has shown that the cornerstone of this communication in our body is found in the intestinal microbiota, which is what influences these interactions. But why is the microbiota important?
Because the interaction between the microbiota and the brain-gut axis appears to be bidirectional, that is, there is communication from the brain to the microbiota and vice versa through neural, endocrine, immune and humoral links.
Microbiome, Microbiota and Meta-genome, Who are they?
Although the terms microbiome and microbiota are used interchangeably, it should be specified that the microbiota is the set of living microbes throughout our body and in greater numbers in the intestinal flora; while microbiome refers to the entire universe of microbes in our body and their genes .
The intestinal microbiota has evolved with humans until today, living in a symbiotic relationship and containing the different populations present in the large intestine that include bacteria, protozoa and viruses.
The metagenome, on the other hand, refers to the genes of microorganisms present in a specific environment such as the microbiota and the collective functions of said microbial genes.
The microbes in our digestive system affect everything in our bodies, from our physical and mental health to our vulnerability to disease.

The bacteria in the microbiome help digest food, regulate the immune system, protect against other bacteria that attack the body, and produce vitamins including vitamins B12, thiamine and riboflavin, as well as vitamin K, which is needed for blood clotting.
At the brain level, the autonomic system with the sympathetic and parasympathetic branches directs the signals that travel through the intestine to the Central Nervous System (CNS) and from the CNS to the intestine. The hypothalamic-pituitary-adrenal (HPA) axis is considered the central axis of stress of any type and is located in the area of the brain that involves memory and emotional responses. Environmental stress, as well as elevated proinflammatory cytokines, activate this system, which, through a process involving the pituitary gland, leads to the release of cortisol from the adrenal glands.
The study publishing these findings also points out that this complex communication system not only ensures the proper maintenance of gastrointestinal homeostasis, but is likely to have multiple effects on affect, motivation and higher cognitive functions.
An imbalance in the gut can have effects on anxiety, depressive behaviors, as well as autism.
The most important link between the gut and the brain is the vagus nerve, which controls salivation, heart rate, and digestion. In turn, the gut responds to the brain by saying, “I am satisfied, I feel good,” or through a calm heart rate, “I am calm.”
The messages that the vagus nerve receives come from metabolites located in the intestinal flora and from messenger substances from the immune and hormonal cells of the intestine.
What Happens When Your Body's Microbiome Is Out of Balance

We all have microorganisms living inside us and we only become aware of them when we have a stomach ache, an infection, an allergy.
Today, science indicates that our individual microbial universe is interwoven with a spectrum of conditions including acne, allergies, obesity, anxiety, cardiovascular disease, irritable bowel syndrome, autoimmune diseases such as diabetes, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, fibromyalgia and even cancer as a result of microbiome dysfunction.
Microbes that attack the body accumulate over time, changing genetic activity and metabolic processes that eventually result in an abnormal immune response against substances and tissues that are normally present in the body.
Take the case of dairy intolerance: initially, the person does not have an allergy or discomfort when consuming them, but excessive ingestion causes a proliferation of harmful bacteria that, eventually, when the person ingests them through food, stomach inflammation, flatulence, nasal congestion and in some cases, a skin reaction, do not take long to occur.
Autoimmune Diseases Are Believed to Be Inherited, Not Through DNA, But Through the Family Microbiome . ( 1 )
There is strong evidence that the colon microbiome differs between obese and lean twins. Obese twins have lower bacterial diversity and higher levels of enzymes, meaning they are more efficient at ingesting food and harvesting calories. Obesity has also been linked to lower microbial diversity in the colon.
Type 1 diabetes is an autoimmune disease associated with a less diverse gut microbiome. In animal studies, the bacteria plays a crucial role in the development of diabetes.
Dust in homes with dogs is believed to reduce the immune response to allergens and other asthma triggers by changing the composition of the gut microbiome. Children who live in homes with dogs have been found to be less likely to develop childhood allergies .
My Favorite Tactics for Maintaining a Healthy Gut

- If you want to get off to a good start, it might be a good idea to do a purge or detox, or at the very least, practice some form of intermittent fasting.

- Take a course of probiotics (30-45 days) to help repopulate the gut with good bacteria. This will strengthen you on several levels:
- Digestive because a healthy colon allows you to better absorb the foods you eat and the nutrients they contain.
- Strengthens the immune system. 70% of the body's immune cells are found in the gut; the probiotic Bifidobacteria infantis alone has been shown to increase T cells that help prevent autoimmune diseases and chronic inflammation.
Likewise, it protects and/or reduces the symptoms and duration of flu and colds.
It can reduce the severity of certain allergies and even eczema or dermatitis.
Note: In addition to probiotic supplements, some foods that contain probiotics include sauerkraut, Kimchi (an oriental preparation of fermented vegetables), Miso (fermented soybeans), Kefir (unsweetened, of course), and Kombucha.
- Mental and emotional . Bacteria in the gut produce neurotransmitters that help promote sleep quality, mood, stress management, anxiety management, and cognitive function.

- Add prebiotic foods to your diet, especially on non-fasting days, which are those that feed the good bacteria already in your intestine in order to strengthen them.
Plus, prebiotics have their own added benefits to further encourage you to include them in your diet:
- Colon bacteria begin to feed on the prebiotic fibers and are able to produce short-chain fatty acids. Among them, butyric acid, which provides balance and regulation to electrolyte levels in the body, while increasing the resistance of the intestinal lining.
- Prebiotics participate in hormonal health by acting as an adaptogenic compound that regulates the release of cortisol (stress hormone).
- Prebiotics may help increase bone density by facilitating the production and bioavailability of several vitamins and minerals such as calcium, iron and magnesium.
The main prebiotic foods
Caution: Prebiotics may cause bloating and gas in some people, so start with small amounts and preferably cooked as they seem to be less tolerated when eaten raw.
Foods rich in prebiotics:
Artichokes, Nori seaweed, cruciferous vegetables such as kale, broccoli, cauliflower; berries, asparagus, red onion, leeks, apples, Konjac root or glucomannan, jicama; cocoa powder, flax seeds, radish, coconut and coconut flour; sweet potatoes, hemp seeds and cabbage.